|
HOW DOES MEDICARE COVER THERAPEUTIC SHOES?
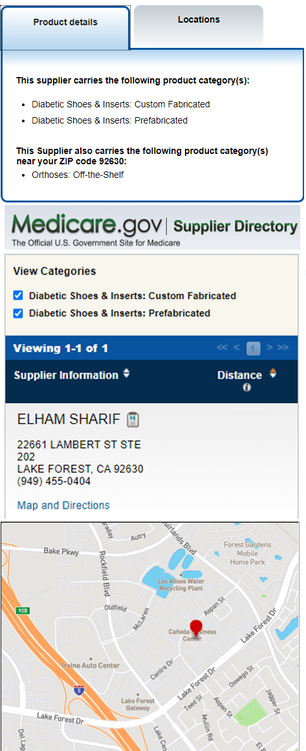
Medicare Part B (Medical Insurance) covers the furnishing and fitting of either one pair of custom-molded shoes and inserts or one pair of extra-depth shoes each calendar year. Medicare also covers 2 additional pairs of inserts each calendar year for custom-molded shoes and 3 pairs of inserts each calendar year for extra-depth shoes. Medicare will cover shoe modifications instead of inserts. Who's eligible? All people with Part B who have diabetes and severe diabetic foot disease are covered. Your doctor must certify that you need therapeutic shoes or inserts. Your costs in Original Medicare If your supplier accepts assignment, you pay 20% of the Medicare-approved amount, and the Part B deductibleapplies. Medicare will only cover your therapeutic shoes if your doctors and suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare. If your doctors or suppliers aren't enrolled, Medicare won't pay the claims submitted by them. It's also important to ask your suppliers if they participate in Medicare before you get therapeutic shoes. If suppliers are participating suppliers, they must accept assignment. If suppliers are enrolled in Medicare but aren't "participating," they may choose not to accept assignment. If suppliers don't accept assignment, there's no limit on the amount they can charge you. Medicare.gov |